Did you know that atherosclerosis (plaque build-up in the arteries) is actually a pediatric disease?
Plaque build-up usually begins during childhood as a fatty streak. It is caused by some initial injury to the inside of the blood vessel wall. Over time, the fatty streak develops into a complex collection of cells called “plaque” that can rupture and block blood flow through the artery. Autopsies of young U.S. service members who died during combat have identified severe atherosclerosis (>50% blockage in at least one blood vessel) in men as young as their twenties and thirties (1).
So if you think that this doesn’t apply to you, I encourage you to think again.
Cardiovascular disease is the leading cause of death for all American men and women today. If you haven’t personally dealt with it, chances are that you know someone who has.
Optimal prevention of heart disease begins early in life.
So, let’s take a look inside the arteries and see how to keep them functioning at their best.
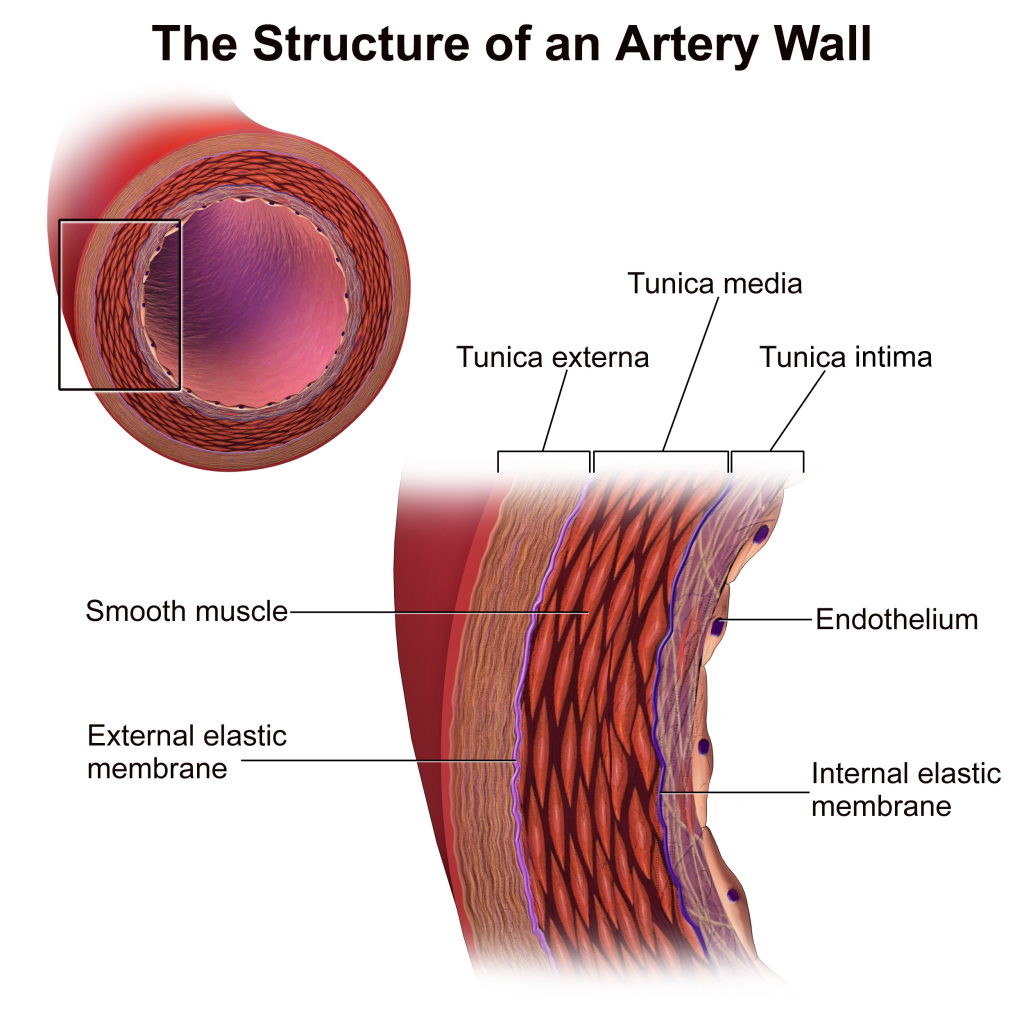
The Anatomy of an Artery
Your arteries transport blood from your heart to all of the cells of your body. They deliver oxygen and nutrients that are necessary to keep you alive. The arteries have a layer of smooth muscle that helps them to open (dilate) and close (constrict). The inside of the arteries are lined with a delicate layer of endothelial cells– collectively called the endothelium.
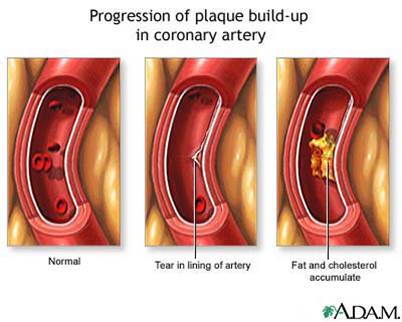
The damage occurs
The problem arises when there is an initial injury to the endothelium. For example, high blood pressure, high blood cholesterol (oxidized LDL), and tobacco can lead to inflammation and endothelial cell damage.
Plaque develops
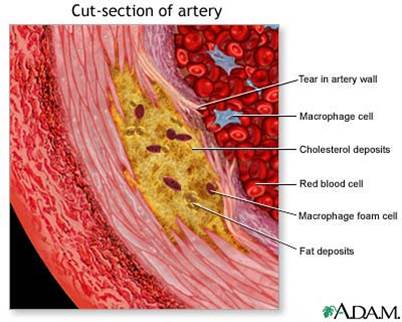
Over time, other cells and substances collect at the site of injury, such as macrophages, LDL cholesterol, white blood cells, fibrinogen, smooth muscle cells, scar tissue, and calcium. A low-level systemic inflammation causes both plaque formation and progression. The body perceives an attack and is desperately trying to defend itself.
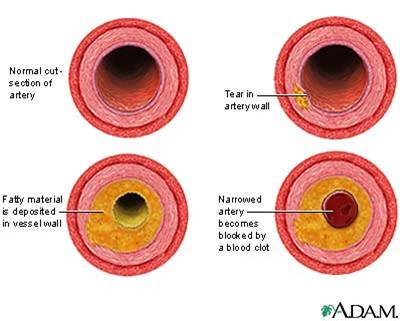
Plaque accumulates and blocks blood flow
Initially, plaque may push the wall of the artery outward. This makes it very difficult to detect and may not cause symptoms for many years. Eventually the plaque grows inward and restricts blood flow through the artery.
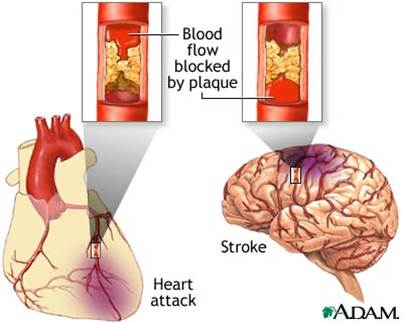
Plaque build up can lead to heart attack or stroke
If a coronary artery that supplies the heart with blood becomes obstructed, then a heart attack occurs. It may cause chest discomfort or pain that radiates down one or both arms, the back, neck, jaw, or stomach. Shortness of breath, nausea, and lightheadedness may also occur.
If a carotid or cerebral artery that supplies the brain with blood becomes obstructed, then a stroke occurs. Symptoms may include facial drooping, arm weakness, and speech difficulty.
When these signs and symptoms are present, it is important to call 9-1-1 immediately so blood can be restored to the affected area.
For more information about the signs and symptoms of a heart attack, click here.
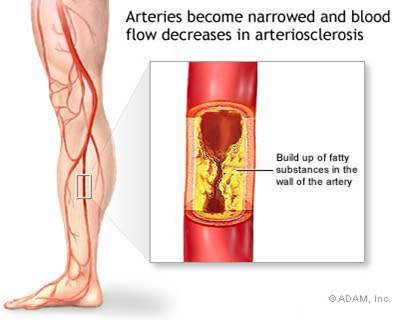
Peripheral Artery Disease occurs when blood vessels in the legs (e.g., femoral or popliteal arteries) become blocked with plaque build up. This restricts blood flow to the calf muscles and can cause pain in the lower legs, particularly during exercise.
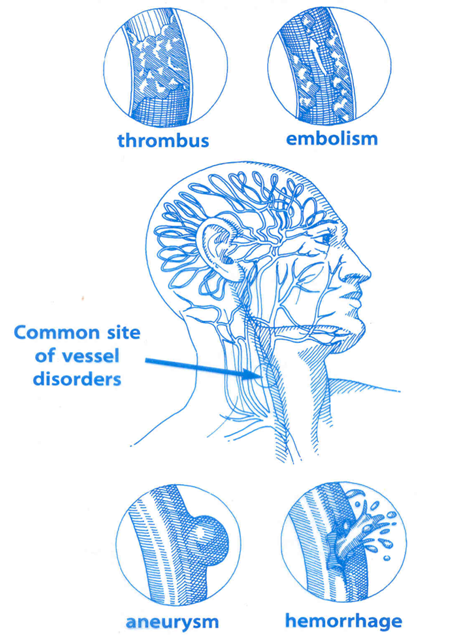
Other blood vessel disorders
There are various types of blood vessel disorders that can occur. A thrombus is a stationary clot. An embolism is a floating clot that may get caught and obstruct blood flow. An aneurysm is a ballooned outward section of a blood vessel wall that may eventually hemorrhage (break).
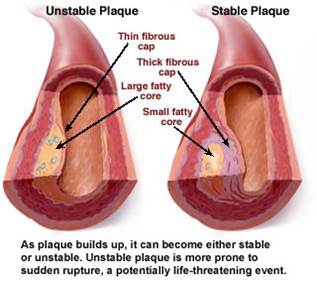
Younger plaques are more likely to rupture
A common misconception is that heart attacks only occur when the plaque builds up enough to completely block blood flow. The truth is that newer, younger plaques are most likely to rupture. These young plaques are only covered by a thin fibrous cap. When the plaque ruptures, various cells immediately rush to the site of injury and form a clot than can quickly block blood flow.
Almost 75% of plaque ruptures occur in arteries than are less than 50% blocked. They may have previously gone undetected because they never caused any symptoms.
Older plaques are still problematic, but they tend to have thicker fibrous caps that are less prone to rupture.
The Good News: You Can Make a Difference
At this point, you are probably wondering if this detrimental process can be reversed. Thankfully, the answer (and entire purpose of this article) is YES! Arterial plaque is constantly progressing and regressing based on the conditions within the blood vessel. When we make unhealthy food choices, remain sedentary, and smoke, plaque progresses.
Moderate lifestyle changes can halt plaque progression. Intensive lifestyle changes can help to reverse it.
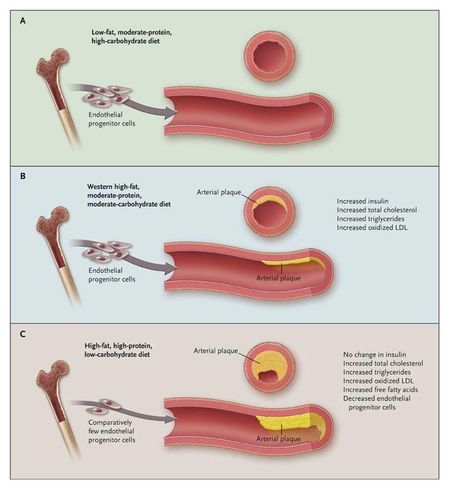
For example, every single bout of exercise causes your body to produce and secrete specialized cells called Endothelial Progenitor Cells (EPCs). These EPCs circulate through your blood vessels, attach to the sites of injury and begin the repair process. Regular exercise is like a constant dose of healing medicine.
Notice in the graphic below that plaque can progress or regress based on the choices that we make every day.
Smith, Steven R. MD. “Clinical Implications of Basic Research. A Look at the Low-Carbohydrate Diet.” N Engl J Med 361(23):2286-88, December 23, 2009
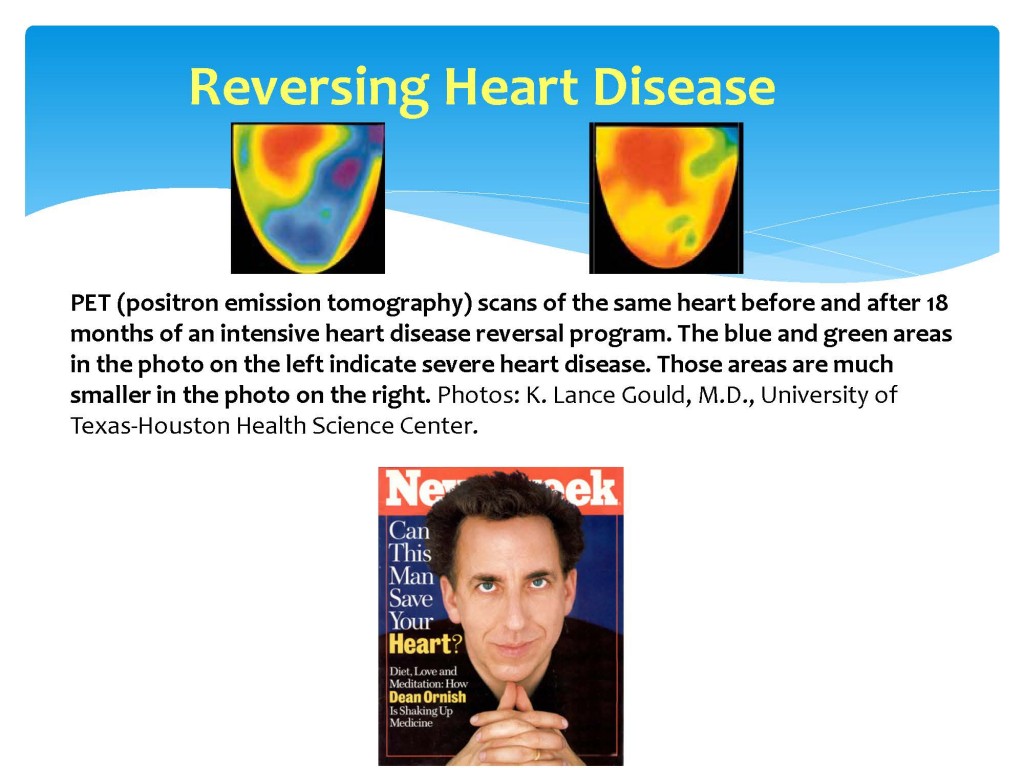
In 1990, cardiologist Dr. Dean Ornish published his classic Lifestyle Heart Trial. He treated patients with Coronary Artery Disease (atherosclerosis in the arteries that supply the heart with blood) with an intensive lifestyle change program. The patients began to walk for exercise, chose a healthful plant-based diet, quit smoking, learned how to manage stress, and received weekly social support. After one year, without any medication or surgery, they experienced regression of plaque build-up (2). Yes, you can heal your heart through lifestyle changes.
To reduce the risk of heart disease, the American Heart Association recommends the following guidelines:
1) Participate in moderate physical activity for at least 30 minutes most, if not all, days of the week.
2) Eat a variety of nutritious foods from many food groups. Emphasize vegetables, fruits, whole grains, and lean sources of protein. Limit red meat.
3) Eat less of the nutrient poor foods. This includes foods such as refined grains, many processed foods, and sugary foods and beverages. Also limit saturated fat, trans fat, and sodium.
4) Don’t use any form of tobacco and avoid secondhand smoke exposure. Smoking can lead to high blood pressure, blood clots, endothelial cell damage, atherosclerosis, heart attack, and stroke.